48year old female
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case I have seen:
Unit II admission on 21/02/2021
DR. YAMINI ( INTERN)
DR. AMULYA ( INTERN)
DR. SURYA PRADEEP ( INTERN)
DR. ASHA KIRAN ( INTERN)
DR. JAYANTH ( INTERN)
DR. VAMSHI ( INTERN)mo
DR. ISMAIL (INTERN)
DR. PRADEEP ( PG 1st YEAR)
DR. NIKITHA ( PG 2nd YEAR)
DR. SUFIYA ( PG 3rd YEAR)
DR. SATISH ( PG 3rd YEAR)
Faculty : DR. VIJAYALAXMI
A 48yr old female came to casualty with
C/O SOB grade 4 since 3:30pm today
C/O uneasiness since 3:30pm today
C/O supra pubic pain since one week ( On and off)
C/O low grade fever with chills since morning
Patient was apparently asymptomatic one week back when she had mild supra pubic tenderness on and off, radiating to right and left lumbar areas, not a/w burning micturition, fever.
Then she developed low grade fever with chills since morning a/w uneasiness, for which she did not take anything orally since 11.00am. When she had SOB grade 4 since 3:30 pm, when she was admitted in nalgonda and diagnosed as DKA(treated with 1000ml of NS)
and Inj HAI (@2ml/hr - 40IU / 40ml NS) and referred here for further management.
History of surgery following RTA with fracture of lumbar Vertebrae in 2016, when she has spine surgery, when she was diagnosed as DM-2 and started on tab. Metformin 500mg
Not a K/C/O HTN, CAD, CVA.
On examinination:
Patient is conscious coherent and cooperative
Tachypneic
Afebrile
RR: 32 cpm
PR: 123 per minute
BP : 110/70 mm Hg
Cvs: S1 S2 heard
RS: Bae positive, coarse end insp crepts left IAA ISA; decreased breath sounds in left IMA
PA: soft nontender BS+
CNS: HMF intact, no FND
Investigations :
HbA1c-6.8%
TROPONIN I- NEGATIVE
LDH- 506 IU/L
HRCT- A)PERIBRONCHIAL AND PREDOMINANTLY CENTRALLY PLACED GROUND GLASS OPACITIES IN BOTH LUNGS
DIFFERENTIALS-
1. INFECTIVE ETIOLOGY(PCP/COVID-19 PNEUMONIA)
2. ACUTE INTERSTITIAL PNEUMONIA
B) CORADS III
C) TOTAL CT SEVERITY SCORE- 24/25
CUE:
ALBUMIN+++, SUGARS+++, PUS CELLS:2-3, EPITHELIAL CELLS:2-3, RED CELLS:2-3
HEMOGRAM- HB:14.5GM%, TLC: 27,400, PLT: 5.8LAKH, N:87, LYM:10, E:2, B:0, PCV:41.4, MCV:79.4, MCHC:35
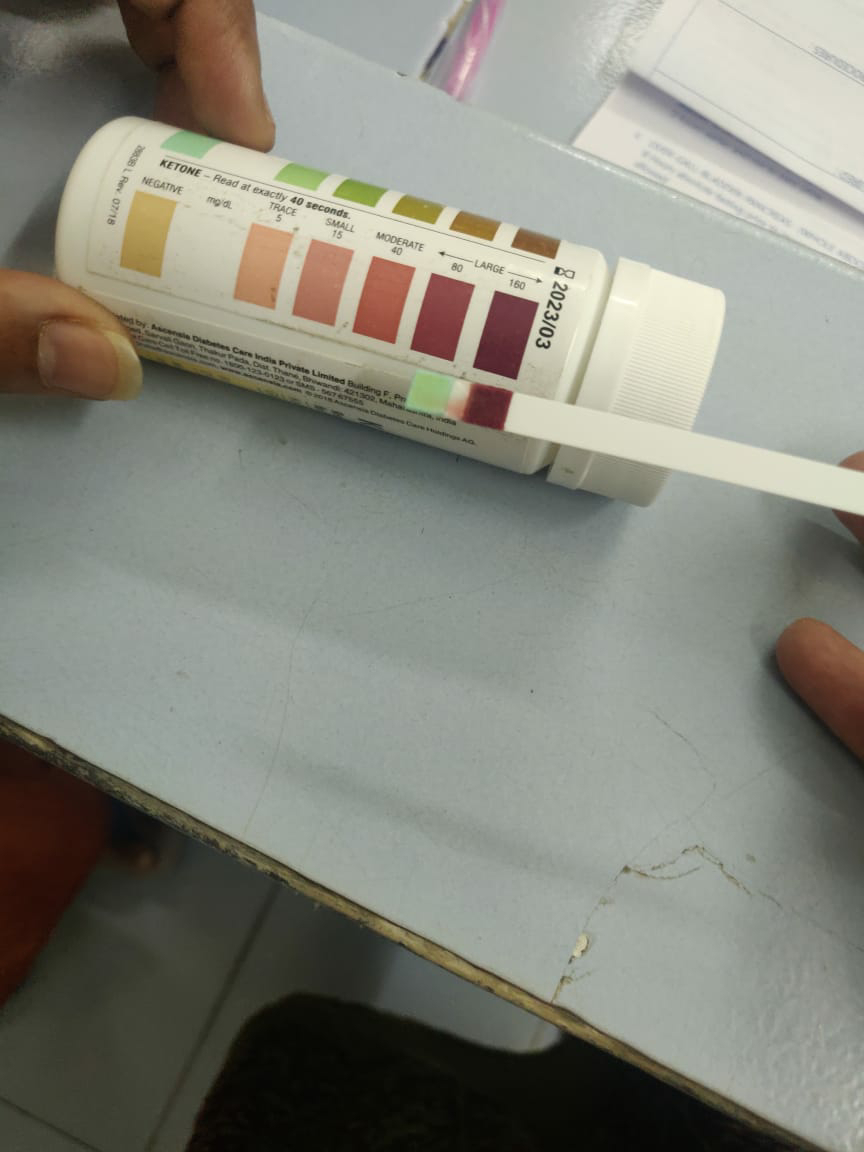
URINE FOR KETONE BODIES- POSITIVE.
SPOT URINE: PROTEIN-31.5
CREATININE- 26.5
RATIO- 1.19
Provisional diagnosis:
K/C/O DM2 with DKA secondary to ?Sepsis
Treatment:
1. INJ NAHCO3 100mEq IV stat
2. NBM till further orders
3. IVF NS(0.9% NaCl) @1000ml/hr for 3 hrs
4. Inj (HAI - 1ml in 39ml NS) @6ml/hr
5. Serum electrolytes and ABG every 4th hrly
6. GRBS hrly monitoring
7. I/O charting hrly
8. INJ MONOCEF 1gm IV BD
9. INJ PANTOP 40mg IV OD
ON DAY 1-22/02/2021
S-
C/O SOB PERSISTENT, NO FEVER SPIKES.
C/O VOMITINGS ONE EPISODE AT 9:00AM.
I/O= 3150/1200ML
O-
O/E PATIENT IS CONCIOUS, COHERENT, COPERATIVE AND ORIENTED TO TIME,
PLACE AND PERSON.
TACHYPNEIC.
AFEBRILE
RR-48CPM
PR-128BPM
BP-130/70MMHG
CVS- S1 S2 PRESENT.
RS- BAE PRESENT, COARSE END INSPIRATORY CREPTS IN LT IAA, ISA,
DECREASED BS IN LT IMA.
PA- SOFT AND NONTENDER, BOWEL SOUNDS PRESENT.
CNS- HMF INTACT, NO FND.
A:
DKA SECONDARY TO PNEUMONIA ?VIRAL ?PSP WITH K/C/O DM II WITH K/C/O
SPINE SURGERY 5YEARS BACK
CARDIOLOGY OPINION TAKEN AND SCREENING ECHO DONE- SHOWED MILD LV
DYSFUNCTION AND LV DILATATION.
ADVISED- HEAD END ELEVATION
INJ. LASIX 20MG IV BD
BI PAP SUPPORT
INJ.CLXAN 0.4ML S/R
ADVICED HRCT I/V/O NON RESOLVING TACHYPNEA AND OPACITIES IN CXR- SHOWED CORADS III
PULMONOLOGY OPINION TAKEN I/V/O TACHYPNOEA AND ADVISED-
SYP.ASCORIL 2TSP TID
T.AZITHROMYCIN 500MG OD
O2 INHALATION 2-4LIT/MIN WITH NASAL PRONGS
SPUTUM C/S CBNAAT AFB
URINE, BLOOD AND SPUTUM C/S
P-
1. ALLOW LIQUIDS AND REGULAR DIET TILL TOLERATED.
2. INJ.PANTOP40MG IV OD.
3. INJ. MONOCEF 1GM IV BD
4. GRBS HRLY.
5. SR ELECTROLYTES AND ABG 4TH HRLY.
6. IVF- 0.45%NS + 5% DEXTROSE(FUSODEX) AT 250ML/HR TILL GRBS <250MG%.
7. INJ. HAI 40IU IN 39ML NS AT 5ML/HR AND INCREASE 1IU IF THERE IS <10% DECREASE IN GRBS AND DECREASE BY 1-2IU/HR WITH >75MG% DECREASE IN GRBS.
8. MAINTAIN GRBS B/W 100-180MG%.
9. INJ.ZOFER 4MG IV TID
10. NEB WITH IPRAVENT 4TH HRLY AND BUDECORT 6TH HRLY
11.INJ. HYDROCORT 100MG IV STAT.
12. AT 11:00PM(22/02/2021) Sr K+=3.1, INJ.KCL 1AMP IN 100ML NS OVER 4HRS.
AT 2:00AM(23/02/2021) Sr K+=3.1, INJ. KCL 1AMP IN 100ML NS OVER 4HRS.
AT 8:00AM(23/02/2021) Sr K+=4.1
ON DAY 2-23/02/2021
S-
C/O SOB DECREASED AND NO FEVER SPIKES, I/O=510F0/1850ML
0-
O/E PATIENT IS C/C/C.
TONGUE IS MOIST AND NO EDEMA.
AFEBRILE
PR- 112BPM
BP- 110/70MMHG ON 10ML/HR INJ. NORAD(8MG) = INJ. DOPAMINE 2ML/HR.
CVS- S1, S2 PRESENT.
RS- BAE PRESENT, END INSPIRATORY COARSE CREPTS PRESENT IN B/L IAA,ISA LT>RT.
SPO2- 97% ON RA.
PA- SOFT, NT, BOWEL SOUNDS PRESENT, PATIENT IS PASSING FLATUS.
CNS- HMF INTACT NO FND.
GRBS- 206MG% ON INJ. HAI INFUSION AT 6ML/HR 40IU.
A-
DKA SECONDARY TO PNEUMONIA ?VIRAL ?PSP WITH K/C/O DM II WITH K/C/O SPINE SURGERY 5YEARS BACK
P-
1. PROPPED UP POSITION.
2. INJ.PANTOP 40MG IV BD.
3. INJ. MONOCEF 2 GM IV BD
4. GRBS HRLY.
5. SR ELECTROLYTES AND ABG 6TH HRLY.
6. INJ. NORAD 8MG IN 46ML NS AT10ML/HR + INJ. DOPAMINE 1AMP IN 50ML NS(200MCG) TO MAINTAIN MAP~65MMHG, TAPER 0.5 ML/HR IF MAP IS MAINTAINING.
7. INJ. HAI 40IU IN 39ML NS AT 5ML/HR AND INCREASE 1IU IF THERE IS <10% DECREASE IN GRBS AND DECREASE BY 1-2IU/HR WITH >75MG% DECREASE IN GRBS.
8. AIR/WATER BED
9. INJ.ZOFER 4MG IV TID
10. NEB WITH IPRAVENT 4TH HRLY.
11.INJ. HYDROCORT 100MG IV OD.
12. INTERMITTENT CPAP VENTILATION 20MINS
13. T. AZITHROMYCIN 500MG PO OD
14. T. TAMIFLU 150MG PO BD.
15. T. BACTRIM-DS 160/800MG OD.
16. INJ. KCL 1AMP IN 100ML NS IV STAT OVER 45 MINS.
Day 3: 24/02/2021
S:
C/O SOB DECREASED AND NO FEVER SPIKES,
NAUSEA DECREASED
O:
PT IS C/C/C
AFEBRILE
PR: 108/MIN NORMAL VOLUME
BP: 90/70MM HG @16ML/HR- NORAD-DS
@4ML/HR- DOPAMINE
CVS: S1 S2 HEARD
RS: BAE POSITIVE NVBS
P/A: SOFT, NON TENDER
RR: 20/MIN
GRBS: 155MG/DL
A-
DKA SECONDARY TO PNEUMONIA ?VIRAL ?PSP WITH K/C/O DM II WITH K/C/O SPINE SURGERY 5YEARS BACK
P:
1. ALLOW REGULAR DIET (DIABETIC)
2. INJ PAN 40MG IV OD
3. INJ MONOCEF 2GM IV BD
4. INJ ZOFER 4MG IV TID
5. INJ HAI S/C 6TH HRLY 15MIN BEFORE MEAL
8AM---2PM---8PM---2AM
6. INJ HYDROCORT 100MG IV OD
7. NEB WITH IPRAVET- 6TH HRLY
8. TAB AZITHROMYCIN 500MG PO OD
9. TAB BACTRIM - DS 160/800MG OD
10. INJ NORAD (8MG IN 46ML/HR @ 16ML/HR)
INJ DOPAMINE ( 1AMP 200MG IN 50ML NS @4ML/HR)
TO MAINTAIN NEARLY 65mm hg
11. IVF NS @UO +30ML/HR
12. OINT THROMBOPHOBE FOR L/A 2ND HRLY
DAY 4: 25/02/2021
S:
C/O SOB DECREASED AND NO FEVER SPIKES,
I/O: 1850ML/3350ML
O:
PT IS C/C/C
AFEBRILE
PR: 97/MIN NORMAL VOLUME
BP: 80/60MM HG @16ML/HR- NORAD-DS
@4ML/HR- DOPAMINE
CVS: S1 S2 HEARD
RS: BAE POSITIVE NVBS
P/A: SOFT, NON TENDER
RR: 20/MIN
A-
DKA SECONDARY TO PNEUMONIA ?VIRAL ?PSP WITH K/C/O DM II WITH K/C/O SPINE SURGERY 5YEARS BACK
P:
1. ALLOW REGULAR DIET (DIABETIC)
2. INJ PAN 40MG IV OD
3. INJ MONOCEF 2GM IV BD
4. INJ ZOFER 4MG IV TID
5. INJ HAI S/C 6TH HRLY 15MIN BEFORE MEAL
8AM---2PM---8PM---2AM
6. INJ HYDROCORT 100MG IV OD
7. NEB WITH IPRAVET- 6TH HRLY
8. TAB AZITHROMYCIN 500MG PO OD
9. TAB BACTRIM - DS 160/800MG OD
10. INJ NORAD (8MG IN 46ML/HR @ 12ML/HR)
INJ DOPAMINE ( 1AMP 200MG IN 46ML NS @1ML/HR)
TO MAINTAIN NEARLY 65mm hg
11. IVF NS @UO +30ML/HR
12. OINT THROMBOPHOBE FOR L/A 2ND HRLY
13. GRBS- 7 POINT
8AM- BBF
10AM- 2HRS AFTER BREAKFAST
1PM- BEFORE LUNCH
3PM- 2HRS AFTER LUNCH
7PM- BEFORE DINNER
9PM- 2HRS AFTER DINNER
2AM
14. INJ 8AM 2PM. 8PM
REGULAR. 16IU. 16IU. 18IU
NPH. 14IU. 14IU
15. INJ 2AMP (40MEQ) KCL IN NS OVER 4HRS
16. SYRUP CREMAFFIN PLUS 15ML/PO. H/S
DAY 5: 26/02/2021
S:
NO C/O SOB AND NO FEVER SPIKES,
PAIN AT CANNULA SITE DECREASED.
I/O: 3900ML/1000ML
O:
PT IS C/C/C
AFEBRILE
PR: 89/MIN NORMAL VOLUME
BP: 90/60MM HG @16ML/HR- NORAD
@4ML/HR- DOPAMINE
CVS: S1 S2 HEARD
RS: BAE POSITIVE NVBS
P/A: SOFT, NON TENDER
RR: 20/MIN
A:
DKA (RESOLVED) SECONDARY TO PCP WITH K/C/O DM2
P:
1. ALLOW REGULAR DIET (DIABETIC)
2. INJ PAN 40MG IV OD
3. INJ MONOCEF 2GM IV BD
4. INJ ZOFER 4MG IV TID
5. INJ HAI S/C 6TH HRLY 15MIN BEFORE MEAL
8AM---2PM---8PM---2AM
6. INJ HYDROCORT 100MG IV OD
7. NEB WITH IPRAVET- 6TH HRLY
8. TAB AZITHROMYCIN 500MG PO OD
9. TAB BACTRIM - DS 160/800MG OD
10. INJ NORAD (8MG IN 46ML/HR @ 12ML/HR)
INJ DOPAMINE ( 1AMP 200MG IN 46ML NS @1ML/HR)
TO MAINTAIN NEARLY 65mm hg
11. IVF NS @UO +30ML/HR
12. OINT THROMBOPHOBE FOR L/A 2ND HRLY
13. GRBS- 7 POINT
8AM- BBF
10AM- 2HRS AFTER BREAKFAST
1PM- BEFORE LUNCH
3PM- 2HRS AFTER LUNCH
7PM- BEFORE DINNER
9PM- 2HRS AFTER DINNER
2AM
14. INJ 8AM 2PM. 8PM
REGULAR. 16IU. 16IU. 18IU
NPH. 14IU. 14IU
15. INJ 2AMP (40MEQ) KCL IN NS OVER 4HRS
16. SYRUP CREMAFFIN PLUS 15ML/PO. H/S











Comments
Post a Comment